CASE REPORT |
https://doi.org/10.5005/jp-journals-10077-3246 |
Oral Health Considerations for the Management of Patients with Junctional Epidermolysis Bullosa
1-3Department of Pediatric and Preventive Dentistry, Kathmandu University School of Medical Sciences (KUSMS), Dhulikhel, Kavre, Nepal
4Department of Pathology, Indira Gandhi Memorial Hospital, Malé, Maldives
5Department of Pediatrics, Hulhumale Hospital, Malé, Maldives
Corresponding Author: Sumita Upadhyay, Department of Pediatric and Preventive Dentistry, Kathmandu University School of Medical Sciences (KUSMS), Dhulikel, Kavre, Nepal, Phone: +977 9841271000, e-mail: drsumipedo@gmail.com
Received on: 03 November 2022; Accepted on: 27 November 2022; Published on: 26 December 2022
ABSTRACT
Epidermolysis bullosa (EB) is a group of hereditary disorders characterized by the mechanical fragility of skin and the appearance of blisters, bullae, and ulcers. This case report presents a 10-year-old boy with junctional EB (JEB) diagnosed at 2 months of age, with skin and oral presentation. There were scar marks of the healed lesion on the forehead, ear, neck, body, palms, and feet. There were no nails in any of the fingers of hands and feet. Ulcers were seen on the lateral border of the tongue, and caries involving pulp were found in three permanent molars. Preventive procedures were performed and root stumps were extracted. Limited mouth opening posed a problem for root canal treatment of permanent molars. Management of EB is challenging and requires a multidisciplinary team approach.
How to cite this article: Upadhyay S, Shrestha R, Dallakoti P, et al. Oral Health Considerations for the Management of Patients with Junctional Epidermolysis Bullosa. J South Asian Assoc Pediatr Dent 2022;5(3):176-179.
Source of support: Nil
Conflict of interest: Dr. Sumita Upadhyay is associated as a member of Editorial Board of this journal and this manuscript was subjected to this journal’s standard review procedures, with this peer review handled independently of the Editor-in-Chief and his research group.
Keywords: Blisters, Bullae, Fragile skin, Junctional epidermolysis bullosa
INTRODUCTION
Epidermolysis bullosa (EB) is a heterogeneous group of rare hereditary disorders characterized by extreme fragility of skin and mucous membrane, which gives rise to the formation of blisters and bullae following minor trauma.1
The tense blisters usually have colorless exudate or hemorrhagic fluid, which leads to eroded areas.
The patient may present with milia, dystrophy or loss of nails, alopecia, exuberant granulation tissue, palmoplantar keratoderma, mottled pigmentation, and pigmented nevi. Secondary skin lesions include cutaneous atrophy, scarring, pigmentary abnormalities, webbing, and contractures due to bullae. These may lead to functional disability.2
The condition occurs due to variations in the gene-encoding proteins of the dermal-epidermal adhesion zone. According to the current classification, the major types of EB are diagnosed based on the level of blister formation; EB simplex, JEB, dystrophic EB, and kindler EB. Further, there are 35 subtypes and five EB-related disorders with skin fragility.3
The diagnosis is based on immunofluorescence mapping and genetic testing,4 which helps in identifying the protein that is altered or missing and the affected gene.
The incidence of inherited EB is around 1:50,000 and the prevalence is 11 cases/million inhabitants.5 The main complications leading to death in children are sepsis, failure to thrive, and respiratory failure.6 Whereas in adults are due to cardiomyopathy, renal failure, and squamous cell carcinoma.7 Pediatric dentists are the first ones to receive the child referred with EB, so they play a very vital role in the early diagnosis and management of the condition. The present paper adds to the report of a case of JEB with clinical features and describes the precautions to be taken during dental treatment.
CASE DESCRIPTION
A 10-year-old boy presented to the Department of Pediatric Dentistry with the chief complaint of decayed teeth in the upper and lower back teeth of the right and left sides of the jaw.
He was a known case of JEB. The history revealed that he developed blisters in all the extremities, face, scalp, and trunk at 2 days of his birth. The parents visited for medical consultation for it and he was diagnosed with JEB after genetic mutation analysis. The details of the analysis were not clearly recorded on the patient’s medical card. Oral blisters were seen at 2 months of age. The fluid-filled blisters developed with minor trauma and were seen in trauma-prone areas of the body. The patient complained of itching of the lesion. The lesion healed with milia and scarring. The systemic lesions were ruled out by investigations. There was no history of similar complaints in the family. The patient had one younger brother who did not have such a condition. He was prescribed oral anti-allergic (hydroxyzine) and aloe vera lotion all over the body.
When the patient presented to our department, on general examination, there were scar marks of the healed lesion on the forehead, ear, neck (collar region), body, palms, and feet (Figs 1 and 2). There were no nails in any of the fingers of the hands and feet (Fig. 2). This was his first dental visit.

Figs 1A to D: Healed lesions with a scar on the forehead, ear, neck, and body

Figs 2A to B: Loss of nails in hands and feet
On intraoral examination, there were ulcerative lesions on the borders of the tongue adjacent to root stumps 75 and 85 (Federation Dentaire Internationale tooth numbering system) (Fig. 3) and in the palate. He had limited mouth opening. There was generalized erythematous marginal and attached gingiva (Fig. 4). Numbers 16, 26, and 36 presented with caries involving pulp, and 46 with dental caries on the occlusal aspect. There were root stumps in relation to 55, 65, 75, and 85. Orthopantomogram was done the assessment of the developing dentition (Fig. 5). The oral hygiene was poor. Informed consent was taken from the patient’s father for recording and reporting the case.

Fig. 3: Microstomia and ulceration in the tongue

Fig. 4: Generalized erythematous gingiva
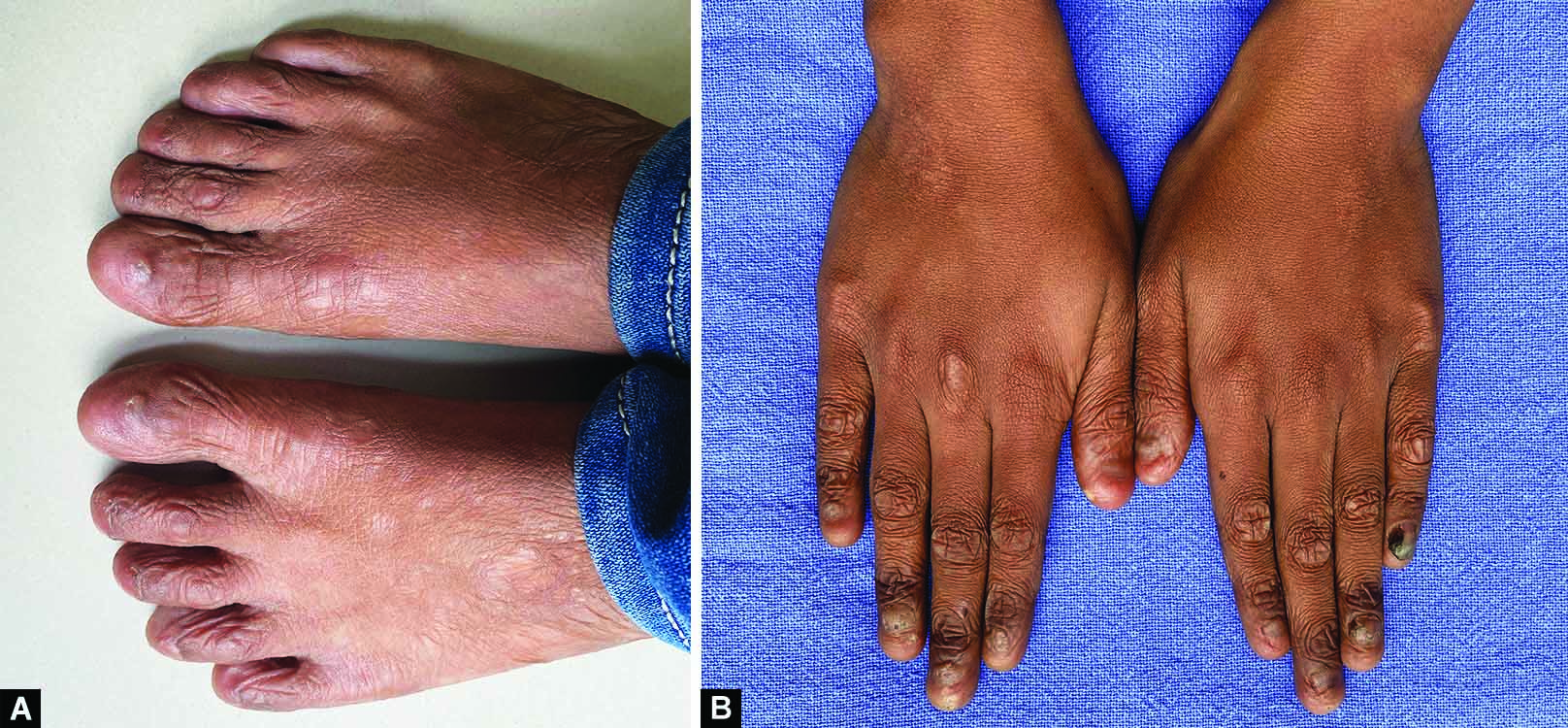
Fig. 5: Orthopantomogram
On the first visit, the patient and parents were given oral hygiene instructions. Oral prophylaxis and fluoride gel application was done. Brushing was advised to be done with a soft-bristled brush and fluoridated toothpaste. In the next two appointments, extraction of 85 was done under local infiltration and 16 and 55 under nerve block. Due to the limited mouth opening, root canal treatment for 16, 26, and 36 could not be done, so it was planned for extraction. Restoration of the other carious teeth was kept in the treatment plan. The patient did not report a new lesion in the follow-up of 1 week. The patient did not attend further follow-up appointments, so the treatment could not be completed.
DISCUSSION
The remarkable feature of EB is the mechanical fragility of the skin and the appearance of blisters and bullae. Patients with EB can present systemic complications, such as ocular, genital, and oropharyngeal infections, involving difficulty in swallowing. However, the patient in the present case did not have systemic complications.
In a research done on 216 patients with EB, perioral and oral granulation tissue lesions were reported in patients with JEB, those tended to resolve during or after adolescence, and all the patients reported with JEB presented microstomia.8 Carroll et al. reported fewer mucosal lesions on examination of patients with JEB.9 However, the present case had mucosal lesions as well as scarred lesions.
Junctional EB (JEB) may have enamel hypoplasia, the diagnosis of which can be done in early referral.10 Wright et al. reported generalized hypoplasia with either severe pitting and/or thin enamel in all JEB cases but not in any other EB types.11 In the present case, except for the permanent mandibular first molar, all other permanent molars were severely affected by caries. The hypoplastic teeth, along with poor oral hygiene, could have been the predisposing factor for such a condition.
The dental care for these patients is affected as they cannot do self-care of their oral cavity. The intraoral painful lesions may also lead to nutritional compromise.12 The management of the cases with EB requires a multidisciplinary approach. They should be referred to pediatric dentists immediately after diagnosis, maybe at around 3–6 months, even before the oral lesions have developed and teeth have erupted, as an early referral and close monitoring may help keep the oral cavity healthy. In the first visit, the parents or caretakers should be counseled regarding diet to prevent dental caries, fluorides, the importance of oral hygiene, and oral manifestations that may arise due to EB.10
Patients with mild oral involvement do not require any treatment modifications, but during dental management, extreme precaution should be taken not to produce any local trauma to the tissues. To prevent such trauma, the mucosa should be lubricated with petroleum jelly. During the restoration of teeth, small-sized instruments, short-shaft dental burs, and small-headed handpieces should be used. The restorations should be highly polished. A cautious administration of local anesthesia should be done to prevent blister formation.13 Limited mouth opening poses clinical difficulty in providing dental treatment in such patients.14,15 It may also complicate intubation during general anesthesia.16 The decreased oral aperture can be slightly increased by daily exercise with a wooden spatula,2 mouth trainers, and a threaded acrylic cone.10
As for the therapeutic management of oral bullae and ulcerations, literature has suggested sucralfate suspension helps in reducing the development and duration of oral mucosal blisters, ulcers, and associated pain.17
A recent publication evaluated the use of cord blood platelet gel and low-level laser therapy and found it to reduce the clinical size, pain, and discomfort due to lesions from the 1st day of treatment.18 Mouthwashes and oral gels are also commonly prescribed in patients with EB, which help to relieve the symptoms.10
All patients with EB, including JEB, requires aggressive dental preventive therapy with regular recall visits, which should include frequent professional cleaning and topical fluoride application.
CONCLUSION
Pediatric dentists are the first ones to receive the referral child case of EB with or without oral lesions. All patients with EB should be managed by a multidisciplinary team from the very early stage of diagnosis. As patients with JEB may have an increased risk of cavities due to enamel hypoplasia, clinicians should be attentive to it from the very beginning. Early preventive therapy will definitely improve the quality of life of the affected children.
REFERENCES
1. Siañez-González C, Pezoa-Jares R, Salas-Alanis JC. Congenital epidermolysis bullosa: a review. Actas Dermosifiliogr 2009;100(10):842–856. DOI: 10.1016/S1578-2190(09)70554-2
2. Lanschuetzer CM, Fine J-D, Laimer M, et al. General aspects. In: Fine J-D, Hintner H, eds. Life with Epidermolysis Bullosa (EB). Vienna: Springer Vienna; 2009:1–95.
3. Has C, Bauer JW, Bodemer C, et al. Consensus reclassification of inherited epidermolysis bullosa and other disorders with skin fragility. Br J Dermatol 2020;183(4):614–627. DOI: 10.1111/bjd.18921
4. Has C, Liu L, Bolling MC, et al. Clinical practice guidelines for laboratory diagnosis of epidermolysis bullosa. Br J Dermatol 2020;182(3):574–592. DOI: 10.1111/bjd.18128
5. Fine JD. Epidemiology of inherited epidermolysis bullosa based on incidence and prevalence estimates from the National Epidermolysis Bullosa Registry. JAMA Dermatol 2016;152(11):1231–1238. DOI: 10.1001/jamadermatol.2016.2473
6. Fine JD, Johnson LB, Weiner M, et al. Cause-specific risks of childhood death in inherited epidermolysis bullosa. J Pediatr 2008;152(2):276–280. DOI: 10.1016/j.jpeds.2007.06.039
7. Hon KL, Li JJ, Cheng BL, et al. Age and etiology of childhood epidermolysis bullosa mortality. J Dermatolog Treat 2015;26(2):178–182. DOI: 10.3109/09546634.2014.915002
8. Wright JT, Fine JD, Johnson LB. Oral soft tissues in hereditary epidermolysis bullosa. Oral Surg Oral Med Oral Pathol 1991;71(4):440–446. DOI: 10.1016/0030-4220(91)90426-d
9. Carroll DL, Stephan MJ, Hays GL. Epidermolysis bullosa–review and report of case. J Am Dent Assoc 1983;107(5):749–751. DOI: 10.14219/jada.archive.1983.0322
10. Krämer S, Lucas J, Gamboa F, et al. Clinical practice guidelines: oral health care for children and adults living with epidermolysis bullosa. Spec Care Dentist 2020;40(Suppl 1):3–81. DOI: 10.1111/scd.12511
11. Wright JT, Johnson LB, Fine JD. Development defects of enamel in humans with hereditary epidermolysis bullosa. Arch Oral Biol 1993;38(11):945–955. DOI: 10.1016/0003-9969(93)90107-w
12. Kramer S. General information on epidermolysis bullosa for the oral health care professional. Spec Care Dentist 2020;40:9–12. DOI: 10.1111/scd.12511
13. Nazir N, Chalkoo AH. Oral manifestations of a patient with epidermolysis bullosa. Biomed J Sci Tech Res 2017;1(6):1562–1565. DOI: 10.26717/BJSTR.2017.01.000486
14. Peñarrocha-Diago M, Serrano C, Sanchis JM, et al. Placement of endosseous implants in patients with oral epidermolysis bullosa. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2000;90(5):587–590. DOI: 10.1067/moe.2000.110438
15. Oliveira MA, Ortega KL, Martins FM, et al. Recessive dystrophic epidermolysis bullosa–oral rehabilitation using stereolithography and immediate endosseous implants. Spec Care Dent 2010;30(1):23–26. DOI: 10.1111/j.1754-4505.2009.00117.x
16. George M, Martinez AE, Mellerio JE, et al. Maxillary alveolar process fracture complicating intubation in a patient with epidermolysis bullosa. Pediatr Anaesth 2009;19(7):706–707. DOI: 10.1111/j.1460-9592.2009.02995.x
17. Marini I, Vecchiet F. Sucralfate: a help during oral management in patients with epidermolysis bullosa. J Periodontol 2001;72(5):691–695. DOI: 10.1902/jop.2001.72.5.691
18. Sindici E, Astesano S, Fazio L, et al. Treatment of oral lesions in dystrophic epidermolysis bullosa: a case series of cord blood platelet gel and low-level laser therapy. Acta Derm Venereol 2017;97(3):383–384. DOI: 10.2340/00015555-2512
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.