REVIEW ARTICLE | https://doi.org/10.5005/jp-journals-10077-3070 |
Contemporary Behavior Guidance Techniques to Outsmart Child’s Anxious Mind
1–3,5Department of Pediatric and Preventive Dentistry, Sudha Rustagi College of Dental Sciences and Research, Faridabad, Haryana, India
4Department of Pedodontics and Preventive Dentistry, Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India
Corresponding Author: Disha Kapil, Department of Pediatric and Preventive Dentistry, Sudha Rustagi College of Dental Sciences and Research, Faridabad, Haryana, India, Phone: +91 9818552236, e-mail: dishakapil.95@gmail.com
How to cite this article Kapil D, Saraf BG, Sheoran N, et al. Contemporary Behavior Guidance Techniques to Outsmart Child’s Anxious Mind. J South Asian Assoc Pediatr Dent 2021;4(1):41–49.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Behavior guidance techniques have been the foundation stone behind success in pediatric dental practice involving both nonpharmacological and pharmacological methods. Modern approaches, attitudes, and expectations of parents and society have devised the modifications in old behavior guidance techniques. However, the applicability of these modalities has not been explored currently. These techniques principally emphasize alleviation of dental anxiety or dentophobia among infants, children, adolescents, and children with special health care needs (SHCN) to provide quality oral health care and to instill a positive dental attitude. This review is intended to provide updates in contemporary behavior guidance techniques such as tell-play-do, animal-assisted therapy, virtual reality, etc., which may provide state-of-art dental management in young children benefitting dental health care providers, parents, and other concerned parties.
Keywords: Child behavior, Dental anxiety, Dental fear and anxiety, Pediatric dentistry..
INTRODUCTION
A child’s dental anxiety and dental phobia stereotypically develop from multiple reasons like a dental drill, air rotor sounds, fear of needles, history of bad dental experience, the smell of dental clinic, and pain (Fig. 1).1 All these situations lead to ignorance and avoidance of dental maintenance, which results in reduced demand for pediatric dental care. “McElroy” in 1895 has beautifully stated that “although operative dentistry may be perfect, the appointment is a failure if a child departs in tears,” stressing the importance of behavior shaping over technical excellence in pediatric dentistry. Avoidance and negligence lead to further complications and give birth to “vicious cycle of Dental Fear” (Fig. 2).2 So, to enhance the dental care, proper planning with the selection of particular techniques and tailoring it according to the needs of an individual parent and skills of the dentist is important. Behavior guidance is a clinical art form of providing safe and effective treatment and skills built on a foundation of science to modify the child’s behavior. A basic understanding of the social, emotional, and cognitive development of the child is very important to perform the specific behavior guidance techniques.3 To maintain compatibility with modern parenting style and child’s attitude with upcoming advanced technologies, the conventional behavior guidance techniques are modified. The focus of these modifications helps to alleviate a child’s dental anxiety and fear, to cultivate a positive dental attitude with the importance of oral health needs, and allowance to perform quality oral health care safely.4
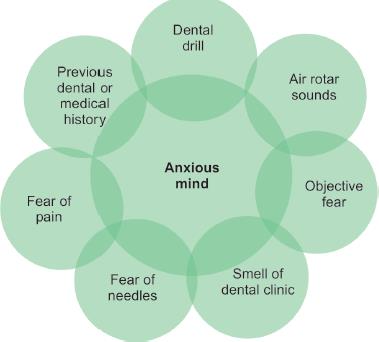
Fig. 1:: Causes of child's dental anxiety
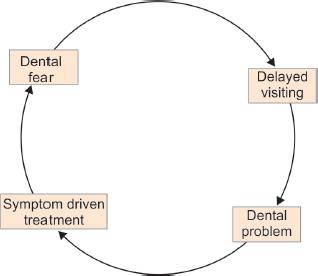
Fig. 2:: Vicious cycle of dental fear
The first dental visit experience plays a vital role in altering the positive dental attitude in children for rendering quality dental treatment in further dental appointments.5 However effective communication development with the child is important owing to this, role plays and pretend play models have been proved to be very effective in engaging a child’s attention. With this idea, a behavior-shaping technique such as tell-show-do has been modified into tell-play-do using concepts of active learning by doing through a playful technique to reduce fear and anxiety in a child.6 Moreover, the fields of robotics and artificial intelligence have been dominating health care, therefore instead a pediatric dentist using conventional methods of behavior guidance may apply this technology in shaping the child’s behavior. All these techniques can be performed in a combination of two or more or individually based upon a benefit vs risk evaluation. As part of the process, parents also play an important role in decision making regarding the treatment and type of technique. With an informed consent (other than communicative guidance), the procedure must be explained to parents with suitable understanding and acceptance.7 Adequate evidence in the scientific literature regarding the knowledge and applicability of recent modifications of behavior guidance techniques in pediatric dentistry is lacking.
Thus, a narrative review is proposed to introduce recent updates in nonpharmacological contemporary behavior guidance techniques that can be efficiently used in the dental office to improve the quality of dental treatment for children.
DATA SOURCE
The main objective of this review article is to collaborate all the advancements and updates in nonpharmacological behavior guidance techniques and provide evidence-based information to support these methods. Data have been collected from five electronic databases: PubMed index, EBSCO, Scopus, the web of science, and Google Scholar from 2010 to 2020 December, using the terms: dental anxiety, contemporary behavior guidance, updates in behavior guidance techniques, nonpharmacological behavior management in pediatric dentistry, animal-assisted dentistry covering the nonpharmacological behavior guidance techniques, original research, and systematic review articles were included for data extraction (Flowchart 1 and Table 1).
Inclusion Criteria
- Abstract available in English.
- Recent and updated behavior guidance techniques published from January 2010 onward.
- Children from 3 to 12 years were included, as the majority of problem occurs during this age group while performing a treatment.
Exclusion Criteria
- Abstract Other than English
- Data regarding pharmacological behavior guidance techniques, meta-analysis, and conventional behavior guidance techniques of the past 10 years.
- Anxiety in children with special healthcare needs and behavior guidance techniques applicable in them.
MODIFIED BEHAVIOR GUIDANCE TECHNIQUES
Tell-Show-Do
This technique of behavior shaping is used by many pediatric dentists; it involves a verbal explanation of what is about to happen in procedure with instruments that will be used (tell), followed by the demonstrations of the procedure by application of visual, tactile, olfactory, and auditory aspects carefully and pleasantly (show), and then (do), initiated by completion of a procedure without deviating from explanation and demonstration.43 Various modifications of the concept of tell-show-do have been introduced recently.
Tell-Play-Do (TPD)
Vishwakarma et al., in 2017, introduced the application of customized dental imitating playing dental objects like a syringe, air rotary, and a cartoon character with mouth wide open in the dental operatory.24 The setup was arranged in the playroom for children to perform dental procedures on it. This made the child to understand the basic dental framework and to become more comfortable with actual dental procedures with a decrease in anxiety levels. He found that TPD was more effective than live modeling on the child’s dental anxiety among the 5–7 years’ age group.

Flowchart 1:: Results of search
| Authors | Date | Study design | Type of technique | Age (in years) | Sample size | Instrument to measure anxiety and fear |
|---|---|---|---|---|---|---|
| Mifflin, Hackmann, Chorney8 | 2012 | Randomized controlled clinical trial | Video distraction | 2–10 | 89 | Modified Yale Preoperative Anxiety Scale |
| Aminabadi et al.9 | 2014 | Randomized controlled clinical trial | Virtual reality | 4–6 | 60 | Wong Baker FACES Pain Rating Scale and state anxiety was measured by Faces version of the Modified Child Dental Anxiety Scale (MCDAS) |
| Singh et al.10 | 2014 | Randomized controlled clinical trial | Audio distraction | 6–12 | 60 | Venham’s picture test, pulse rate, blood pressure, and oxygen saturation |
| Naithani, Viswanath11 | 2014 | Comparative study | Audiovisual distraction (nursery rhymes and cartoons in English or regional language) | 4–8 | 75 | Venham Picture Test (VPT), Venham Rating of Clinical Anxiety (VRCA), Child Fear Survey Schedule (CFSS), Pulse Rate and Oxygen Saturation |
| Paryab, Arab5 | 2014 | Randomized clinical trial study | Tell-show-do (filmed modeling) | 4–6 | 46 | Venham and Frankl rating scales, heart rate |
| Alrshah, Kalla, Abdellatif6 | 2014 | Randomized clinical trial study | Live modeling vs. tell-show-do | 6–9 | 120 | The vital sign and facial image scale |
| Dedeepya et al.12 | 2014 | Randomized controlled clinical trial | Biofeedback | 9–13 | 40 | Biofeedback system (heart rate (HR), skin conductance (SC), blood volume pulse (BVP), temperature, electromyography (EMG), and electroencephalography), visual analog scale |
| Nuvvula et al.13 | 2015 | Randomized controlled clinical trial | Audiovisual distraction with 3D video glasses | 7–10 | 90 | MCDAS(f) (self-report), pulse rate (physiological), behavior (using Wright’s modification of Frankl behavior rating scale and Houpt scale) |
| Attar, Baghdadi14 | 2015 | Randomized controlled clinical trial | iPad vs audiovisual eyeglasses | 4–8 | 42 | The Modified Dental Anxiety Scale (MDAS), the Wong-Baker FACES Pain Rating Scale (FACES), the North Carolina Behaviour Rating Scale, pulse oximeter |
| Navit et al.15 | 2015 | Randomized controlled clinical trial | Audio distraction aids (MP3 player, headphones and audio MP3 files of popular movie songs, instrumental music, nursery rhymes, and children stories) | 6–12 | 150 | The Venham’s Picture Test (VPT), Venham’s Clinical Rating Scale (VCRS), and pulse rate measurement with the help of pulse oximeter |
| Kaur et al.1 | 2015 | Randomized controlled clinical trial | Audio and audiovisual distraction | 4–8 and 6–8 | 60 | Heart rate—fingertip pulse oximeter, dental subscale of children fear survey schedule—short-scale eight-item questionnaire, clinical anxiety rating scale, and cooperative behavioral rating scale |
| Sayed et al.16 | 2016 | Randomized controlled clinical trial | Live display video output of the DOM (dental operating microscope) displayed on a 72-inch LCD monitor | 7–9 | 90 | The dental operating microscope, pulse oximeter, Venham’s picture test |
| Al-Khotani, Bello, Christidis17 | 2016 | Randomized controlled clinical trial | Audiovisual distraction | 7–9 | 56 | The Facial Image Scale (FIS) and the modified Venham’s clinical ratings of anxiety and cooperative behavior scale (MVARS). The vital signs, blood pressure, and pulse |
| Chaturvedi et al.18 | 2016 | Randomized controlled clinical trial | Audiovisual distraction eyeglasses | 6–10 | 40 | Wong-Bakers Faces Pain Rating Scale, Visual Analog Scale (VAS), and pulse oximeter |
| Allani, Setty19 | 2016 | Randomized controlled clinical trial | Distraction (playing video game on the mobile phone and viewing videos of patient’s favorite cartoon character on mobile phone) | 4–8 | 60 | Facial image scale through a questionnaire |
| Yasemin et al.20 | 2016 | Randomized controlled clinical trial | Distraction (humanoid robots) | 4–10 | 33 | Frankl’s Behaviour Rating Scale (FBRS), Facial Image Scale (FIS), pulse oximeter |
| Babaji et al.21 | 2017 | Randomized controlled trial | Different colored apron, formal dress, and cartoon character along with conventional syringe and camouflage syringe with a toy-like appearance | 6–14 | 400 | Modified Child Dental Anxiety Scale faces version |
| Rank et al.22 | 2017 | Randomized controlled trial | Distraction (toys and children stories) | 4–6 | 62 | Facial Image Scale (FIS) and the Behavior Rating Scale (BRS) |
| Shah et al.23 | 2017 | Randomized controlled trial | Smartphone applications (Kid Dentist App) vs traditional behavior management techniques | 5–10 | 60 | Blood pressure, oxygen saturation (SaO2), facial anxiety scale |
| Vishwakarma et al.24 | 2017 | Randomized controlled trial | Customized tell-play-do (TPD) technique | 5–7 | 98 | Heart rate, Facial Image Scale (FIS), and Venham six-point index |
| Habib-Agahi et al.25 | 2017 | Randomized controlled clinical trial | Telescopic dental needles | 4–8 | 50 | Sound, eye, motor (SEM) scale, face version of visual analog scale (VAS) |
| Gupta, Gupta, Gupta26 | 2017 | Randomized controlled clinical trial | Relaxing music distraction | 3–7 | 60 | Venham picture test, North Carolina behavior rating scale, and visual analog scale |
| Al-Halabi , Bshara, AlNerabieah27 | 2018 | Randomized clinical trial | Inferior alveolar nerve administrated with using AV eyeglasses ‘VR Box’ and wireless headphone and using tablet device and wireless headphones | 6–10 | 102 | Wong–Baker FACES (self-report), pulse rate (physiological) and behavior (using FLACC behavior rating scale (“external evaluator”) |
| Garrocho-Rangel et al.28 | 2018 | Crossover randomized and controlled clinical trial | Video Eyeglasses/Earphones System (VEES) | 5–8 | 40 | The Face, Legs, Activity, Cry, Consolability (FLACC) scale. Pulse rate and oxygen saturation measurements |
| Atzori et al.29 | 2018 | Randomized controlled clinical trial | Virtual reality distraction in an Oculus Rift VR helmet | Mean age 13.20 years old | 5 | Children self-rated their “worst pain,” “pain unpleasantness,” “time spent thinking about pain,” “presence in VR,” “fun,” and “nausea” levels during the dental procedures, using graphic rating scales |
| Meshki et al.30 | 2018 | A preliminary double-blind randomized clinical trial | Interactive modeling using computer games (smartphone dental simulation game) | 4–7 | 50 | The Wong-Baker Facial Rating Scale (W-BFRS), heart rate |
| Niharika et al.31 | 2018 | Randomized single-blind-controlled clinical trial | Virtual reality eyeglasses | 4–8 | 40 | Wong–Baker FACES Pain Rating Scale and state anxiety was measured by Faces version of the Modified Child Dental Anxiety Scale (MCDAS). Changes in pulse oximeter and heart rate were recorded in every 10 minutes |
| Khandelwal et al.32 | 2018 | Randomized controlled study | “Tell-show- do” method and audiovisual distraction | 5–8 | 400 | Facial image scale (FIS), Venham’s picture test (VPT), blood pressure, pulse rate (PR), and oxygen saturation (SpO2) at different stages of the visit |
| Shahnavaz et al.33 | 2018 | Open-trial | Internet-based cognitive behavioral therapy | 8–15 | 18 | Visual analog scale (VAS; no fear-strong fear) and the fear scale; Children’s Fear Survey Schedule-Dental Subscale (CFSS-DS), diagnostic instrument K-SADS-PL |
| Berge et al.34 | 2018 | Randomized controlled clinical trial | Cognitive behavioral therapy | 10–16 | 67 | Psychometric self-report scales: Intraoral injection fear scale (IOIF-s), Children’s Fear Survey Schedule-Dental Subscale (CFSS-DS), Injection Phobia Scale for children (IS-c), and Mutilation Questionnaire for children (MQ-c) and a behavioral avoidance test (BAT) followed by a questionnaire |
| Nammalwar, Rangeeth35 | 2018 | Randomized controlled clinical trial | Animal-assisted activity | 4–11 | 20 | Questionnaires, using a modified pictorial scale (RMS Pictorial Scale) |
| Monika et al.36 | 2019 | Randomized controlled clinical trial | Camouflaged (CaS) and conventional syringe (CoS) | 6–8 | 80 | Venham Picture Test (VPT) and Face, Leg, Activity, Cry and Constability (FLACC) Behavioral Pain Assessment Scale |
| Shetty, Suresh, Hegde37 | 2019 | Randomized controlled clinical trial | Virtual reality | 5–8 | 120 | Modified Child Dental Anxiety Scale, Wong Baker Faces pain rating scale, Salivary cortisol levels |
| Bux, Porritt, Marshman38 | 2019 | Randomized controlled clinical trial | Self-Help Cognitive Behavioural Therapy | 8–16 | 84 | Children’s Experiences of Dental Anxiety Measure (CEDAM) |
| Radhakrishna et al.39 | 2019 | Randomized controlled clinical trial | Group I: Tell-show-play-doh; Group II: smartphone dentist game; and Group III: Tell-show-do technique | 4–8 | 60 | Pulse rate, Facial Image Scale (FIS), Frankl’s behavior rating scale, and FLACC (Face, Leg, Activity, Cry, Consolability) behavior scales |
| Khandelwal, Shetty, Rath40 | 2019 | Randomized controlled clinical trial | Group I was termed as the control group; in group II, the audio distraction technique was used. Group III received audio–video distraction (AVD) by means of a chair-mounted audio–video device, and group IV received AVD by means of a ceiling-mounted television. | 4–10 | 80 | RMS pictorial scale (RMS-PS), Venham picture test (VPT), pulse rate, oxygen saturation |
| Vallakatla et al.41 | 2020 | Randomized controlled clinical trial | Camouflage sleeves of two colors green and pink, with decorative stickers | 4–14 | 24 | Wong-Baker Faces pain scale, Venham picture test (VPT) |
| Kasimoglu et al.42 | 2020 | Randomized controlled clinical trial | Techno-psychological distraction technique (humanoid robot) | 4–10 | 200 | Parental Corah Dental Anxiety Scale, Facial Image Scale (FIS), physiological pulse rate. and Frankl Behaviour Rating Scale (FBRS) |

Fig. 3:: Tell-show-play-do

Fig. 4:: Smart phone dentist app

Fig. 5:: Dog therapy
Tell–Show-Play-Doh
The most commonly used method in pediatric dentistry tell-show-do was modified into the tell-show-play-doh technique by Radhakrishna et al. in 2019.39 The battery-operated “Play-Doh Doctor Drill ‘n Fill toy” set was introduced to play and familiarize them with dental setup consisting of suction, air rotor, and air-water syringe. This idea of modification, learning by doing on dental imitation toy with euphemisms, helped the children to alleviate anxiety, constructed a bond for future communication, and aided in improved dental treatment with quality (Fig. 3).
Distraction
Distraction techniques involve the strategies that overload the patient’s limited attention capacity, thus diverting their attention from unpleasant dental treatment44 in which several types of distraction techniques (3D eyeglasses,13 biofeedback,12 children’s stories, and toys,22 dental operating microscope,16 nursery rhymes, live modeling, virtual reality eyeglasses,45 use of camouflaged syringes,21,36,41 and telescopic needles25) were included. They concluded it as a good strategy for the management of anxious and fearful children without any contraindication.
Smart Phone Dentist App
The forthcoming advancements in technology have also entered the dentistry sphere. Patel et al. in 2017 and Meshki et al. in 2018 introduced the Android application dentist games to reduce dental fear and to make comfortable and aware of the dental procedures and idea of the performance of treatment.30,46,47 The dentist application was downloaded days before the treatment on the parent’s Android phone and virtually allowed the children to play the game. These games are approved by a panel of experienced pedodontists for demonstrating the clinical procedure like brushing, oral prophylaxis, restorations, and extractions, etc., giving the clinical effects with sounds categorize in different levels to reach the complete healthy mouth at the end (Fig. 4).
Animal-assisted Activity
Animal-assisted activities (AAA) can be a great adjunct to practice in the dental office with appropriately trained and qualified dogs according to the infection control guidelines and potential health risks. Shiloh et al. in 2003 revealed that petting a live animal over a toy animal reduced self-reported anxiety.48 Moreover, Barker et al. in 200349 verified that interaction with a live animal for just 15 minutes significantly reduced anxiety and fear when compared to the control group of children who read magazines. Comparison of the anxiety level of children between 4 years and 11 years by introducing the therapy dog in the waiting area and operatory area showed a significant reduction in levels of stress hormones, such as cortisol, adrenaline, and norepinephrine.35 Also, AAAs have been found as a complementary intervention in reducing pain and its related symptoms, anxiety, depression, and loneliness in the medical field. However, more studies are needed to be done in dental offices in India for stronger evidence50 (Fig. 5).
Music Therapy
Audiotaped music connected to headphones works as the distraction technique, which showed a reduction in both biological and psychological anxiety levels. In 2012, Spintge et al. suggested a positive result in the moderation of pain, stress, and anxiety by music therapy.51 Also, in 2014 Singh et al. exhibited a decrease in intraoperative anxiety levels by listening to self-selected music between 6-year and 12-year olds undergoing extraction.10 Whereas on the contrary, Gupta et al. in 2017 concluded that music did not significantly reduce pain, anxiety, or disruptive behavior between 3-year and 7-year olds who required treatment under local analgesia.26 This concluded the indecisive and partial quality of evidence in support of reducing dental anxiety in children with music therapy and the need for more evidence-based study for a more significant result.52,53
Audiovisual Distraction
It has been thought that distraction should be able to involve visual, auditory, and kinesthetic sensory modalities and active participation of the child. The focus of the child is diverted from unpleasantness and to engage them with specific visual and audio effects with imagination. Audiovisual distraction (AVD) was modified from the audio distraction technique and demonstrated a more significant result. Various ways of AVD techniques such as iPads and tablets have been presented with a moderate type of anxiety, which has been shown to alleviate anxiety and comfort children during anesthesia induction, immunization shots, and wart cryotherapy.8,54-56 In 2016, Chaturvedi et al. conducted a study on comparative evaluation with and without AVD eyeglasses and found an iPad-based video delivery system to decrease anxiety before cast room procedures in 6–10-year-old children.18
Television (Chair or Ceiling Mounted)
Khandelwal et al. (2018) concluded that the AVD technique by using cartoons and animated video clips on the laptop was more effective than tell-show-do and more beneficial if both the techniques are combined.32 Ceiling-mounted AVD was found to be the most effective in reducing anxiety followed by chair-mounted AVD as compared to audio distraction40 (Fig. 6).
Active Video Games
According to Allani et al. in 2016, an active video game or cartoon video on a mobile phone involves the visual, mental, and motor participation of the child that would help to reduce anxiety preoperatively.19 However, evidence applying this method in pediatric dentistry has been lacking.
Virtual Reality
Virtual reality (VR) technology constructs the computer-simulated environment with the use of a head-mounted display (HMD) that covers the eyes with an optical lens and two separate displays. This allows the patient to virtually experience an immersive, simulated visual, and auditory scenario to be in that world by withholding sensory information from the real world.29 Thus, VR has a substantial good effect during dental procedures because it breaks the negative cycles of past bad dental experiences and enhances the positive experiences resulting in overall successful dental treatment.57
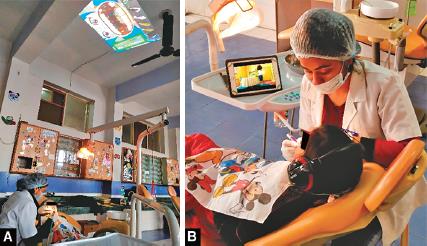
Figs 6A and B:: Audiovisual distraction
Humanoid Robots
Yasemin et al. in 2016 introduced a techno-psychological distraction technique by using a humanoid robot—“IRobi.”20,42 Such modification of the conventional distraction technique to distraction by humanoid robots with the multisensory system supporting videos, audio-based dialogues, expression, and gestures with bodily movement showed greater impact in distracting child and enabling them to feel less pain while treatment. This combination of audio, visual, and tactile stimuli with advanced technology where robots are superior to people in contact with children made a comfortable environment for both dentists and children. This novel technique too requires to be conducted and texted in the Asian subcontinent.
Virtual Reality Box
Al-Halabi et al. in 2018 demonstrated that video shown on tablet devices connected to headphones worked best over VR box in alleviating anxiety and pain during administration of inferior alveolar nerve block between 6-year and 10-year olds.27 They also concluded that VR box to be more acceptable in older patients between 8- and 10-year-old children with an additive positive attitude for the next dental visits.
Virtual Reality Eyeglasses
The VR device (Google VR Box and Anti-Tank Virtual Reality 3D Glasses) connected to the cartoon series “Doraemon” was endorsed to children undergoing pulp therapy by Niharika et al. in 2018.31 These VR eyeglasses connected to headphones to provide the sound blocked the visual field of the child completely and made them in that virtual world. This technique is very effective in modulating pain and anxiety by letting the patient get to detach from viewing the dental procedures, instruments, and hearing of sounds of air rotor, making them unaware of what is happening in the environment. A similar study by Custódio et al. in 2020 substantiated it as an effective tool for improving behavior and reducing pain perception during the dental treatment of children.58
Cognitive Behavior Therapy
Cognitive-behavioral therapy (CBT) is based on the concept that molds negative thoughts and feelings into parts to think in a positive way to manage current problems and behave accordingly. This medicine is used for psychiatric conditions that provide psychoeducation, techniques to cope up, and cognitive restructuring. Berge et al. (2017) evaluated the effect of five sessions of CBT for 10–16 years olds with intraoral injection phobia. This showed significant positive results in alleviation of dental phobia when compared to the control group.34 Cognitive behavior therapy produces better anxiety reduction than diverse behavioral guidance techniques but requires stronger evidence-based studies in pediatric dentistry for its effective application.59 Bux et al. (2019) conducted the guided self-help CBT resources “Your teeth, you are in control” service with children aged between 8 and 16 years who had self-reported dental anxiety on their initial examination appointment. This evaluation indicated an effective and child-centered approach in reducing child dental anxiety.38 Convenience to perform CBT face to face had become difficult because of limited time availability and long distances to the pediatric dental clinic with a lack of psychologists at the clinic. However, to overcome this loophole the cognitive behavioral therapy is reconstructed to Internet-based CBT for making easy accessibility with advanced technology.33,60
CONCLUSION
As we are heading toward the modern world with the adoption and proliferation of digital communication technology widely in every field, a shifting paradigm has evoked the need to reconstruct the old conventional behavior guidance techniques with miraculous advancements for patient care in the smart digital era.
REFERENCES
1. Kaur R, Jindal R, Dua R, et al. Comparative evaluation of the effectiveness of audio and audiovisual distraction aids in the management of anxious pediatric dental patients. J Indian Soc Pedodont Prevent Dent 2015;33(3):192. DOI: 10.4103/0970-4388.160357.
2. Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: Exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health 2007;7(1):1. DOI: 10.1186/1472-6831-7-1.
3. Oliver K, Manton DJ. Contemporary behavior management techniques in clinical pediatric dentistry: out with the old and in with the new? J Dent Child 2015;82(1):22–28.
4. Swarna K, Prathima GS, Suganya M, et al. Recent advances in non-pharmacological behaviour management techniques in children–an overview. IOSR J dent Med Sci 2019;18:18–21.
5. Paryab M, Arab Z. The effect of filmed modeling on the anxious and cooperative behavior of 4-6 years old children during dental treatment: a randomized clinical trial study. Dent Res J 2014;11(4):502.
6. Alrshah SA, Kalla IH, Abdellatif AM. Live modelling vs tell-show-do technique for behaviour management of children in the first dental visit. Mansoura J Dent 2014;1(3):72–77.
7. American Academy of Pediatric Dentistry. Behavior guidance for the pediatric dental patient. The Reference Manual of Pediatric Dentistry. Chicago, Ill: American Academy of Pediatric Dentistry; 2020. pp.292–310. Assessed on November 2, 2020.
8. Mifflin KA, Hackmann T, Chorney JM. Streamed video clips to reduce anxiety in children during inhaled induction of anesthesia. Anesth Analg 2012;115(5):1162–1167. DOI: 10.1213/ANE.0b013e31824d5224.
9. Aminabadi NA, Erfanparast L, Sohrabi A, et al. The impact of virtual reality distraction on pain and anxiety during dental treatment in 4-6 year-old children: a randomized controlled clinical trial. J Dent Res Dent Clin Dent Prospects 2012;6(4):117.
10. Singh D, Samadi F, Jaiswal JN, et al. Stress reduction through audio distraction in anxious pediatric dental patients: an adjunctive clinical study. Int J Clin Pediatr Dent 2014;7(3):149. DOI: 10.5005/jp-journals-10005-1254.
11. Naithani M, Viswanath D. Child’s dental anxiety: management by audio and audio-visual distraction technique-a comparative study. Univ Res J Dent 2014;4(2):1–01. DOI: 10.4103/2249-9725.132974.
12. Dedeepya P, Nuvvula S, Kamatham R, et al. Behavioural and physiological outcomes of biofeedback therapy on dental anxiety of children undergoing restorations: a randomised controlled trial. Eur Archi Paediat Dentis 2014;15(2):97–103. DOI: 10.1007/s40368-013-0070-3.
13. Nuvvula S, Alahari S, Kamatham R, et al. Effect of audiovisual distraction with 3D video glasses on dental anxiety of children experiencing administration of local analgesia: a randomised clinical trial. Eur Archi Paediat Dentis 2015;16(1):43–50. DOI: 10.1007/s40368-014-0145-9.
14. Attar RH, Baghdadi ZD. Comparative efficacy of active and passive distraction during restorative treatment in children using an iPad versus audiovisual eyeglasses: a randomised controlled trial. Eur Archi Paediat Dentis 2015;16(1):1–8. DOI: 10.1007/s40368-014-0136-x.
15. Navit S, Johri N, Khan SA, et al. Effectiveness and comparison of various audio distraction aids in management of anxious dental paediatric patients. J Clin Diagnos Res: JCDR 2015;9(12):ZC05. DOI: 10.7860/JCDR/2015/15564.6910.
16. Sayed A, Ranna V, Padawe D, et al. Effect of the video output of the dental operating microscope on anxiety levels in a pediatric population during restorative procedures. J Indian Soc Pedodont Prevent Dentis 2016;34(1):60–64. DOI: 10.4103/0970-4388.175516.
17. Al-Khotani A, Bello LA, Christidis N. Effects of audiovisual distraction on children’s behaviour during dental treatment: a randomized controlled clinical trial. Acta Odontol Scand 2016;74(6):494–501. DOI: 10.1080/00016357.2016.1206211.
18. Chaturvedi S, Walimbe H, Karekar P, et al. Comparative evaluation of anxiety level during the conventional dental procedures with and without audiovisual distraction eyeglasses in pediatric dental patients. Journal of International Oral Health 2016;8(11):1016.
19. Allani S, Setty JV. Effectiveness of distraction techniques in the management of anxious children in the dental operatory. IOSR J Dent Med Sci 2016;15(10):69–73. DOI: 10.9790/0853-1510026973.
20. Yasemin M, Kasımoglu Y, Kocaaydın S, et al. Reduction of dental anxiety and pain in children using robots. In Proceedings from the Ninth International Conference on Advances in Computer-Human Interactions 2016 Apr 24.Assessed on November 2, 2020.
21. Babaji P, Chauhan PP, Rathod V, et al. Evaluation of child preference for dentist attire and usage of camouflage syringe in reduction of anxiety. Eur J Dentis 2017;11(4):531. DOI: 10.4103/ejd.ejd_223_17.
22. Rank RC, Rank MS, Vilela JE, et al. Dental anxiety and behavior in young children undergoing different distraction techniques. Pesquisa Brasileira em Odontopediatria e Clínica Integrada 2017;17(1):3651.
23. Shah HA, Nanjunda Swamy KV, Kulkarni S, et al. Evaluation of dental anxiety and hemodynamic changes (Sympatho-adrenal response) during various dental procedures using smartphone applications v/s traditional behaviour management techniques in pediatric patients. Int J Appl Res 2017;3:429–433.
24. Vishwakarma AP, Bondarde PA, Patil SB, et al. Effectiveness of two different behavioral modification techniques among 5–7-year-old children: a randomized controlled trial. J Indian Soc Pedodont Prevent Dent 2017;35(2):143. DOI: 10.4103/JISPPD.JISPPD_257_16.
25. Habib-Agahi R, Gandjalikhan-Nassab SA, Hashemipour MA, et al. Comparing pain and pain-related behavior in children with invented telescopic dental needles. J Oral Health Oral Epidemiol 2017;6(1):33–39.
26. Gupta N, Gupta H, Gupta P. Evaluation of the role of music as a nonpharmacological technique in management of child patients. J Contemp Dent Pract 2017;18(3):194–197. DOI: 10.5005/jp-journals-10024-2015.
27. Al-Halabi MN, Bshara N, AlNerabieah Z. Effectiveness of audio visual distraction using virtual reality eyeglasses versus tablet device in child behavioral management during inferior alveolar nerve block. Anaesth, Pain Intens Care 2018. 55–61.
28. Garrocho-Rangel A, Ibarra-Gutiérrez E, Rosales-Bérber M, et al. A video eyeglasses/Earphones system as distracting method during dental treatment in children: a crossover randomised and controlled clinical trial. Eur J Paediat Dentis 2018;19(1):74–79.
29. Atzori B, Lauro Grotto R, Giugni A, et al. Virtual reality analgesia for pediatric dental patients. Front Psychol 2018;9:2265. DOI: 10.3389/fpsyg.2018.02265.
30. Patil VH, Vaid K, Gokhale NS, et al. Evaluation of effectiveness of dental apps in management of child behaviour: a pilot study. Int J Pedodon Rehabilitat 2017;2(1):14. DOI: 10.4103/ijpr.ijpr_5_17.
31. Niharika P, Reddy NV, Srujana P, et al. Effects of distraction using virtual reality technology on pain perception and anxiety levels in children during pulp therapy of primary molars. J Indian Soc Pedodont Prevent Dent 2018;36(4):364. DOI: 10.4103/JISPPD.JISPPD_1158_17.
32. Khandelwal D, Kalra N, Tyagi R, et al. Control of anxiety in pediatric patients using “Tell show do” method and Audiovisual distraction. J Contemp Dent Pract 2018;19(9):1058–1064. DOI: 10.5005/jp-journals-10024-2381.
33. Shahnavaz S, Hedman-Lagerlöf E, Hasselblad T, et al. Internet-based cognitive behavioral therapy for children and adolescents with dental anxiety: Open trial. J Med Internet Res 2018;20(1):e12. DOI: 10.2196/jmir.7803.
34. Berge KG, Agdal ML, Vika M, et al. Treatment of intra-oral injection phobia: a randomized delayed intervention controlled trial among Norwegian 10-to 16-year-olds. Acta Odontol Scand 2017;75(4):294–301. DOI: 10.1080/00016357.2017.1297849.
35. Nammalwar RB, Rangeeth P. A bite out of anxiety: evaluation of animal-assisted activity on anxiety in children attending a pediatric dental outpatient unit. J Indian Soc Pedodont Prevent Dent 2018;36(2):181. DOI: 10.4103/JISPPD.JISPPD_54_18.
36. Monika K, Poonacha KS, Anshula D, et al. Comparative evaluation of dental anxiety and fear in children by using Camouflaged syringe and conventional syringe. J Dental Sci 2019;4(1):000214.
37. Shetty V, Suresh LR, Hegde AM. Effect of virtual reality distraction on pain and anxiety during dental treatment in 5 to 8 year old children. J Clin Pediat Dentist 2019;43(2):97–102. DOI: 10.17796/1053-4625-43.2.5.
38. Bux S, Porritt J, Marshman Z. Evaluation of self-help cognitive behavioural therapy for children’s dental anxiety in general dental practice. Dentistry journal 2019;7(2):36. DOI: 10.3390/dj7020036.
39. Radhakrishna S, Srinivasan I, Setty JV, et al. Comparison of three behavior modification techniques for management of anxious children aged 4–8 years. J Dent Anesth Pain Med 2019;19(1):29–36. DOI: 10.17245/jdapm.2019.19.1.29.
40. Khandelwal M, Shetty RM, Rath S. Effectiveness of distraction techniques in Managing pediatric dental patients. Int J Clin Pediatr Dent 2019;12(1):18. DOI: 10.5005/jp-journals-10005-1582.
41. Vallakatla V, Vallakatla S, Dutta S, et al. Conventional and camouflage syringe during Maxillary dental procedures: Relevance to anxiety and pain levels in children. Biomedical and Pharmacology Journal 2020;13(1):253–258. DOI: 10.13005/bpj/1883.
42. Kasimoglu Y, Kocaaydin S, Karsli E, et al. Robotic approach to the reduction of dental anxiety in children. Acta Odontol Scand 2020;78(6):474–480. DOI: 10.1080/00016357.2020.1800084.
43. Armfield JM, Heaton LJ. Management of fear and anxiety in the dental clinic: a review. Aust Dent J 2013;58(4):390–407. DOI: 10.1111/adj.12118.
44. Prado IM, Carcavalli L, Abreu LG, et al. Use of distraction techniques for the management of anxiety and fear in paediatric dental practice: a systematic review of randomized controlled trials. Int J Paediatr Dent 2019;29(5):650–668. DOI: 10.1111/ipd.12499.
45. Ghadimi S, Estaki Z, Rahbar P, et al. Effect of visual distraction on children’s anxiety during dental treatment: a crossover randomized clinical trial. Eur Archi Paediat Dentis 2018;19(4):239–244. DOI: 10.1007/s40368-018-0352-x.
46. Meshki R, Basir L, Alidadi F, et al. Effects of pretreatment exposure to dental practice using a smartphone dental simulation game on children’s pain and anxiety: a preliminary double-blind Randomized clinical trial. J Dent 2018;15(4):250.
47. Arias MC, McNeil DW. Smartphone-based exposure treatment for dental phobia: a pilot randomized clinical trial. J Public Health Dent 2020;80(1):23–30. DOI: 10.1111/jphd.12340.
48. Shiloh S, Sorek G, Terkel J. Reduction of state-anxiety by petting animals in a controlled laboratory experiment. Anxiety Stress Coping 2003;16(4):387–395.
49. Barker SB, Pandurangi AK, Best AM. Effects of animal-assisted therapy on patients’ anxiety, fear, and depression before ECT. J ECT 2003;19(1):38–44. DOI: 10.1097/00124509-200303000-00008.
50. Manley L. On the use of pets to manage dental anxiety. Dental Hypotheses 2016;7(3):117. DOI: 10.4103/2155-8213.190518.
51. Spintge R. Clinical Use of Music in Operating Theatres.New York, NY: Oxford University Press; 2012.
52. Arangannal P. Effect of music on pain and anxiety in pediatric dental patients. Indian J Pub Health Res Develop 2019;10(12):1127–1130.
53. Ainscough SL, Windsor L, Tahmassebi JF. A review of the effect of music on dental anxiety in children. Eur Archi Paediat Dentis 2019;20(1):23–26. DOI: 10.1007/s40368-018-0380-6.
54. Shahid R, Benedict C, Mishra S, et al. Using iPads for distraction to reduce pain during immunizations. Clin Pediatr 2015;54(2):145–148. DOI: 10.1177/0009922814548672.
55. Tey HL, Tan ES, Tan FG, et al. Reducing anxiety levels in preschool children undergoing cryotherapy for cutaneous viral wart. Arch Dermatol 2012;148(9):1001–1004. DOI: 10.1001/archdermatol.2012.1656.
56. Zhang C, Qin D, Shen L, et al. Does audiovisual distraction reduce dental anxiety in children under local anesthesia? A systematic review and meta-analysis. Oral Dis 2019;25(2):416–424. DOI: 10.1111/odi.12849.
57. Rosiak J, Szymańska J. Non-pharmacological methods of fighting dental anxiety. J Pre-Clin Clin Res 2018;12(4):145–148. DOI: 10.26444/jpccr/99771.
58. Custódio NB, Costa FD, Cademartori MG, et al. Effectiveness of virtual reality glasses as a distraction for children during dental care. Pediatr Dent 2020;42(2):93–102.
59. Gomes HS, Viana KA, Batista AC, et al. Cognitive behaviour therapy for anxious paediatric dental patients: a systematic review. Int J Paediatr Dent 2018;28(5):422–431. DOI: 10.1111/ipd.12405.
60. Radomski AD, Wozney L, McGrath P, et al. Design and delivery features that may improve the use of internet-based cognitive behavioral therapy for children and adolescents with anxiety: arealist literature synthesis with a persuasive systems design perspective. J Med Internet Res 2019;21(2):e11128. DOI: 10.2196/11128.
________________________
© The Author(s). 2021 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.