CASE REPORT | https://doi.org/10.5005/jp-journals-10077-3038 |
Fragment Reattachment of an Uncomplicated Crown–Root Fracture: A Case Report
1,2Department of Pedodontics and Preventive Dentistry, MA Rangoonwala College of Dental Sciences and Research Centre, Pune, Maharashtra, India
3Anjali Dental Clinic and Dental Speciality Centre, Mumbai, Maharashtra, India
Corresponding Author: Sneha S Kothare, Department of Pedodontics and Preventive Dentistry, MA Rangoonwala College of Dental Sciences and Research Centre, Pune, Maharashtra, India, Phone: +91 9833750115, e-mail: sneha.kothare@yahoo.com
How to cite this article Kothare SS, Choubey S, Das A. Fragment Reattachment of an Uncomplicated Crown–Root Fracture: A Case Report. J South Asian Assoc Pediatr Dent 2020;3(1):30–33.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Traumatic dental injuries are very common in children and adolescents, with the line of treatment depending on the time elapsed, age of the child, and tooth maturity. Management of crown–root fractures is a multidimensional process involving management of the traumatized tooth as well as the adjacent soft tissues. The present case report is of a 10-year-old boy with an uncomplicated crown fracture of permanent maxillary right central incisor and a palatal uncomplicated crown–root fracture of his permanent maxillary left central incisor. Both the teeth were endodontically treated in a two-visit process, and gingivectomy was performed palatally with the left central incisor. The fractured fragment was reattached using nano-filled dual-cure composite resin and tooth restored with composite resin. The fragment showed opaque discoloration that reduced over time but still persisted after 1 year. During the follow-up period, no unfavorable radiographic changes were seen. The prognosis of the teeth was favorable with good esthetic results.
Keywords: Fragment reattachment, Fragment rehydration, Periodontal health, Root fracture, Uncomplicated crown.
INTRODUCTION
Dentoalveolar traumas are very common in children and adolescents, which are mostly caused by falling, fighting, vehicle accidents, and sports. Dental fractures because of trauma usually occur in the maxillary anterior teeth, and these fractures subsequently lead to esthetic, functional, and phonetic problems.
The conventional treatment of uncomplicated crown fracture has been restorations with composite resin and dental bonding systems. However, this treatment modality becomes further complex when the fracture line extends subgingivally.1 The International Association of Dental Traumatology (IADT) guidelines (2013) state that, in such situations, the coronal crown–root segment be removed followed by a gingivectomy, and sometimes ostectomy with osteoplasty, with subsequent endodontic treatment and restoration with a post-retained crown or reattachment of the fractured fragment using composite resin.2 This approach of reattachment has also shown considerable success as reported by Ertugrul et al.1
This case report presents the management of an uncomplicated crown–root fracture of a permanent maxillary left incisor in a 10-year-old boy.
CASE DESCRIPTION
A 10-year-old boy reported to the outpatient department with an uncomplicated crown fracture of permanent maxillary right incisor (11) and an uncomplicated crown–root fracture of his permanent maxillary left incisor (21) with the fractured fragment still attached palatally (Fig. 1).
The patient revealed that the injury was sustained by hitting a flower bed on the playground 15 days ago and that the fractured fragment was mobile since then. There was excessive bleeding from the maxillary gingiva and upper lip immediately after the injury with associated swelling lasting 4–5 days. An attempt was made by the parent to remove the fragment, as it interfered with biting, but was abandoned due to severe pain and bleeding from the affected tooth. There was no episode of unconsciousness or nasal bleed. No medical or dental treatment was sought at this juncture. The patient was self-medicating analgesics for the past 15 days for pain because of the moving fractured fragment on the palatal side of the tooth. No antibiotic therapy was initiated. The medical history of the patient revealed no systemic disease.
Clinical examination showed that the patient had sustained an uncomplicated crown fracture of 11 up to the middle third of the crown and an uncomplicated crown–root fracture of 21 with the fracture line of 21 extending to the coronal third of the root subgingivally from mesiolingual line angle to the junction of middle and distal third of the tooth on the palatal aspect. On the buccal aspect, the fracture line extended into the enamel and dentin up to the middle third of the crown. Mild gingival inflammation was seen associated with palatal gingiva of 21. The fractured fragment showed Miller’s Grade II mobility labiopalatally, while the affected teeth showed Miller’s grade I mobility. There was tenderness on palpation with 11 and 21 due to subluxation. The fragment interfered with occlusion and was retained in the oral cavity with only soft tissue adhesions. Radiographic evaluation revealed no associated alveolar injuries, and root formation of both the affected teeth was complete. It also showed that the subgingival fracture with 21 was extending to the coronal third of the root, while the coronal fracture with 11 involved enamel and dentin only. Periodontal ligament space was widened with respect to 11 and 21. The vitality of the tooth could not be diagnosed clearly by electrical pulp test. No thermal tests were performed. Based on the clinical and radiographic evaluation, the following treatment plans were decided: (1) removal of the fractured fragment, (2) multivisit nonsurgical root canal therapy (NSRCT), (3) gingivectomy with 21, and (4) fragment reattachment and restoration with composite resin. An informed consent was obtained from the parents and assent from the child.

Fig. 1: Uncomplicated crown–root fracture of his permanent maxillary left incisor (21) with the fractured fragment still attached palatally
After application of benzocaine 20% w/v topical anesthetic gel (ProGel-B; Septodont Healthcare India Pvt. Ltd., India) at the injection site, nasopalatine nerve block was administered using 2% lignocaine with epinephrine [Xylofic 2% ADR (1:200,000); Gufic Biosciences Ltd., India], and the mobile tooth fragment was removed (Figs 2A to C). Bleeding was seen from marginal gingiva of 11 distally and from attached gingiva of 21, i.e., 4 mm palatally from the gingival margin. The fragment was cleaned and immediately placed in distilled water. Hemostatic agent (Viscostat Clear; Ultradent Products Inc., USA) was applied to the palatal gingiva subgingivally to control hemorrhage. The affected teeth and one tooth distal to it were cleaned with pumice slurry and splinted using glass-fiber-reinforced composite flexible splint (Interlig; Angelus Industria de Productos Odontologicos S/A, Brazil) for 2 weeks. After splinting, the rubber dam isolation was achieved using split-dam technique and NSRCT was initiated in both teeth. The root canals were minimally prepared using #S2 and #F1 ProTaper Gold (Dentsply Maillefer, USA) rotary files. Copious canal irrigation and disinfection were performed with 1% sodium hypochlorite solution. After the chemomechanical preparation, the canals were dried using absorbent paper points and a nonsetting high pH calcium hydroxide intracanal medicament (Ultracal XS; Ultradent Products Inc., USA) was placed within the canals and the tooth was temporized. Gingivectomy was performed on the palatal aspect of 21 using diode laser (CHEESE II Medical Diode Laser; Wuhan Giga Optronics Technology Co. Ltd., Wuhan, China) at 1.5 Watt power to excise gingiva and expose the subgingival extent of the fracture (Fig. 2D). Care was taken not to damage the incisive papilla. Broad-spectrum antibiotics and analgesics were prescribed to the patient for 5 days and soft diet was advised for 1 week. Oral hygiene instructions were given to the patient but compliance in this regard was poor.
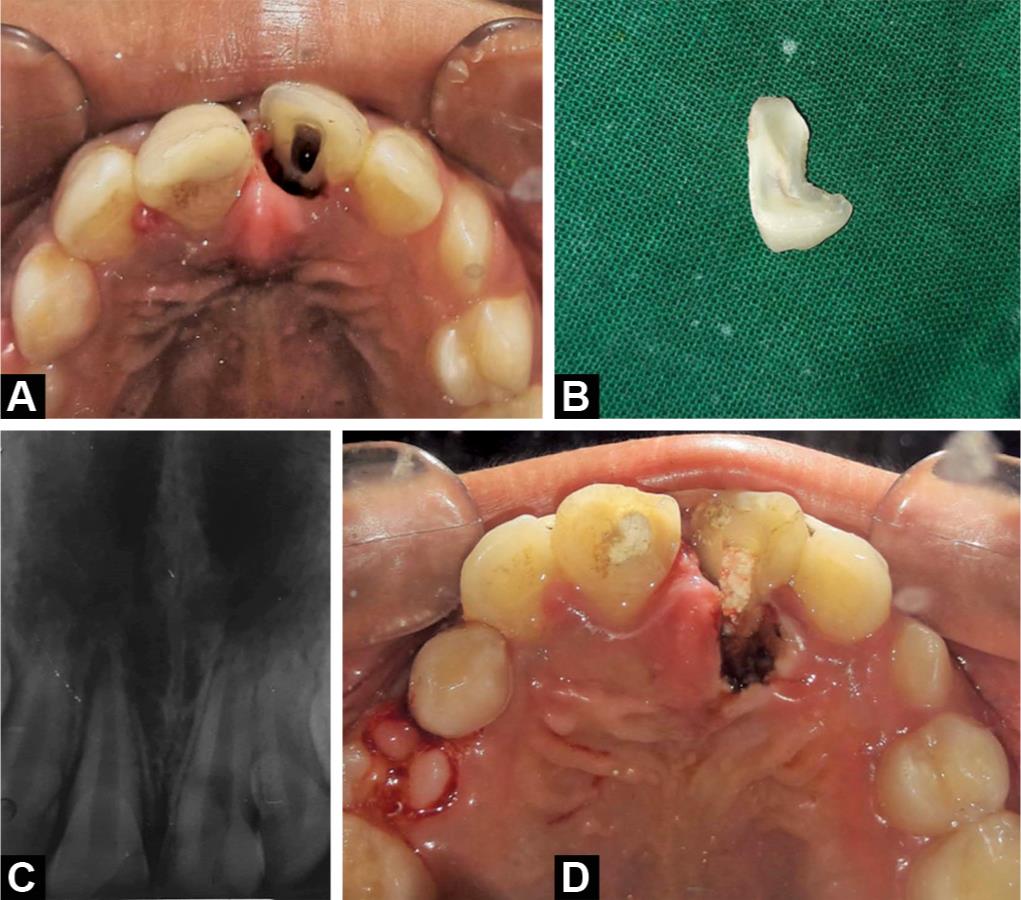
Figs 2A to D: (A) Palatal view of 21 with the fragment removed and access opening done; (B) Separated fragment; (C) Preoperative radiograph of 11, 21; (D) Temporization of 11, 21 and diode laser gingivectomy of palatal aspect of 21
After 1 week, the gingivectomy site showed uneventful healing with adequate exposure of the fracture line. Both the teeth were asymptomatic and were thus obturated using gutta-percha and resin sealer (Fig. 3A). The flexible splint was removed prior to the fragment attachment. The 21 was anesthetized palatally before the reattachment of the fragment. The fragment and the affected tooth were prepared using an incisal double bevel as suggested by Simonsen, against a chamfer which is commonly practiced, without removal of the internal dentin.3 The fragment and the fractured tooth were etched with 35% phosphoric acid gel for 20 seconds, rinsed, and dried. The bonding agent (Single Bond; 3M Espe, Seefeld, Germany) was applied to the etched surfaces and reattached using nano-filled dual-cure composite (LuxaCore Z-Dual; DMG America, USA) including core restoration instead of a flowable composite and light cured for 40 seconds on each side per manufacturer’s recommendations. A dual-cure composite resin was used for improved bonding and higher strength. The attached fragment appeared opaque white as compared to the rest of the tooth. Coronal restoration of 11 was done using A2 dentin, A2 enamel, and incisal shade composite resin (Tetric N-Ceram; Ivoclar Vivadent, India) (Figs 3B and C).
The patient was recalled after 3 months, 6 months, and 1 year and follow-up was done using the core outcome set suggested by Kenny et al.4 At the 3 months’ follow-up, the teeth were asymptomatic and 2 mm gingival recession seen on the palatal aspect of 21 with no periodontal pocket formation. Mild opaque white coloring of the fragment persisted (Fig. 4). After 6 months, the teeth remained asymptomatic and gingival recession reduced to 1 mm palatally with 21 (Fig. 5A). No unfavorable radiographic changes were seen at this point (Fig. 5B). At the end of 12 months, the patient was asymptomatic and the periodontal status was acceptable though the palatal gingival margin of 21 was 1 mm lower than 11. Mild opaque discoloration of the reattached fragment was seen with acceptable facial esthetics and function (Fig. 6). Radiologically, no untoward changes were observed.

Figs 3A to C: (A) NSRCT with 11, 21; (B) Uneventful healing of palatal aspect of 21 and fragment reattachment with 21 after 3 days; (C) Postoperative radiograph of 11, 21 showing the fragment reattachment margin

Figs 4A to C: (A) The 3-month follow-up anterior view of 11, 21; (B) Three-month follow-up palatal view of 11, 21 showing 2 mm gingival recession on the palatal aspect of 21; (C) Three-month follow-up radiograph of 11, 21

Figs 5A and B: (A) The 6-month follow-up palatal view of 11, 21 showing reduction in gingival recession on the palatal aspect of 21 to 1 mm; (B) The 6-month follow-up radiograph of 11, 21 showing no unfavorable radiographic changes
DISCUSSION
In the management of any traumatic dental injury, the time elapsed since the injury is crucial in the decision-making process for treatment. In this case, as the time elapsed, since the injury was 15 days old and the patient was already symptomatic, the endodontic management was initiated immediately and fragment reattachment was deferred till the second appointment. This not only allowed for gingival healing following the gingivectomy but also helped prevent any endodontic flare-up with either teeth.

Fig. 6: The 12-month follow-up of 11, 21 showing mild opaque discoloration of the reattached fragment
Management of a crown–root fracture with subgingival extension is a complex process, but adherence to the IADT guidelines has shown considerable success. However, in this case, the fragment reattachment was done according to the guidelines but the tooth was restored with composite resin only and not a post-retained crown as the majority of the crown structure remained on the alveolar segment of the affected tooth and the crown–root ratio was maintained. Furthermore, a composite resin restoration has a favorable subgingival reaction with the formation of junctional epithelium and connective tissues adjacent to subgingival restorative materials in humans. This also provides good adaptability of the reattached fragment to the tooth with favorable esthetics.1
One of the important aspects to ascertain in the follow-up appointments was the periodontal status in the postoperative period with respect to 21. Minimal bleeding was observed following the gingivectomy in the first appointment. In the subsequent visit, uneventful healing was observed in the region without any pocket formation. It was observed that the 2-mm gingival recession seen on the palatal aspect of the tooth reduced to 1 mm after 6 months. No pocket formation was seen during the follow-up period. This is in accordance with the findings of Eichelsbacher et al. who reported that fragment reattachment using composite resin in periodontally healthy teeth affected by crown–root fractures had no detrimental impact on periodontal health over a period of 2 years.5
In the present case, the reattached fragment appeared opaque white in color due to dehydration immediately after reattachment. This occurs due to dehydration of the dentin which appears to rehydrate in the mouth over time due to absorption of water.6 The fragment did regain its color and translucency over time in this case as well. However, at 1-year follow-up, mild opaque discoloration still persisted but the overall esthetics were acceptable to the patient. And more amount of time may be required for absolute color harmony of the fragment.7
CONCLUSION
Management of a crown–root fracture is a complex and technique-sensitive process that, when undertaken in accordance with the prescribed guidelines, would have a good prognosis with acceptable esthetic results and functions.
AUTHOR DECLARATION
All of the authors have made substantive contribution to this manuscript, and we have reviewed the final paper prior to its submission. We, as authors, guarantee that the article has not been published and is not being considered for publication elsewhere.
REFERENCES
1. Ertugrul F, Eden E, Ilgenli T. Multidiciplinary treatment of complicated subgingivally fractured permanent central incisors: two case reports. Dent Traumatol 2008;24(6):e61–e66. DOI: 10.1111/j.1600-9657.2008.00709.x.
2. DiAngelis AJ, Andreasen JO, Ebeleseder KA, et al. International association of dental Traumatology guidelines for the management of traumatic dental injuries: 1. fractures and luxations of permanent teeth. Dent Traumatol 2012;28(1):2–12. DOI: 10.1111/j.1600-9657.2011.01103.x.
3. Simonsen RJ. Restoration of a fractured central incisor using original tooth fragment. J Am Dent Asso 1982;105(4):646–648. DOI: 10.14219/jada.archive.1982.0436.
4. Kenny KP, Day PF, Sharif MO, et al. What are the important outcomes in traumatic dental injuries? An international approach to the development of a core outcome set. Dent Traumatol 2018;34(1):4–11. DOI: 10.1111/edt.12367.
5. Eichelsbacher F, Denner W, Klaiber B, et al. Periodontal status of teeth with crown–root fractures: results two years after adhesive fragment reattachment. J Clin Periodontol 2009;36(10):905–911. DOI: 10.1111/j.1600-051X.2009.01458.x.
6. Toshihiro K, Rintaro T. Rehydration of crown fragment 1 year after reattachment: a case report. Dent Traumatol 2005;21(5):297–300. DOI: 10.1111/j.1600-9657.2005.00314.x.
7. Yilmaz Y, Guler C, Sahin H, et al. Evaluation of tooth-fragment reattachment: a clinical and laboratory study. Dent Traumatol 2010;26(4):308–314. DOI: 10.1111/j.1600-9657.2010.00907.x.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.