ORIGINAL RESEARCH | https://doi.org/10.5005/jp-journals-10077-3036 |
Assessment of Dietary Behavior Change in Families Participating in a “Two-week Sugar Challenge”: An Observational Study
1,2Department of Pedodontics, Dr. GD POL Foundation’s YMT Dental College and Hospital, Navi Mumbai, Maharashtra, India
Corresponding Author: Ashwin M Jawdekar, Department of Pedodontics, Dr. GD POL Foundation’s YMT Dental College and Hospital, Navi Mumbai, Maharashtra, India, Phone: +91 9821009615, e-mail: jawdekar.ashwin@gmail.com
How to cite this article Manek S, Jawdekar AM. Assessment of Dietary Behavior Change in Families Participating in a “Two-week Sugar Challenge”: An Observational Study. J South Asian Assoc Pediatr Dent 2020;3(1):14–18.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Background: Dietary behaviors are a result of social and cultural practices; consumption of sugar-rich food and beverages being no exception. The World Health Organization (WHO) sugar guideline 2015 states that adults and children should reduce their daily intake of sugar to less than 10% of their total energy and a further reduction to 5% would provide additional health benefits. In view of this, a dietary behavior change pertaining to free-sugar reduction is needed in families.
Aim: To assess the dietary behavior change in families participating in a “2-week sugar challenge” in terms of their willingness to participate and adherence to the challenge and defaults.
Settings and design: A 2-week sugar challenge was conducted in a residential complex in Mumbai.
Materials and methods: This study consisted of a convenient sample of 30 families with children belonging to 3- to 12-year age-group, who were approached for the study. They were given a list of products to be avoided and that could be consumed. Families and individuals were assessed for willingness to participate and adherence to the challenge.
Statistical analysis: Variable means, standard deviations, and percentages were analyzed.
Results: Of the contacted families, more than 80% (with children aged 3–12 years) were willing to participate in the study. Of the participating families, 2.70% and 3.22% of adults and children sustained the challenge for 2 weeks, respectively. None of the families as a whole could adhere to the challenge. The mean number of days the challenge was sustained by adults and children was 2.96 (±3.79) and 3.04 (±3.77), respectively. The most common defaulted food item was “milk additives.”
Conclusion: Willingness in terms of sugar challenge was high but sustainability was poor.
Keywords: Behavior, Diet, Environment, Families, Obesity, Parents.
INTRODUCTION
Dental caries and obesity are widely prevalent in children.1 A common risk factor approach is the need of the hour to tackle this situation, where dental caries has several impacts on quality of life, and obesity may predispose to noncommunicable diseases later.2,3 Dietary behavior change is considered difficult and changing environment is the key to such a behavior change.4 Targeting families as units for inculcating dietary behaviors could be necessary for sustenance of behavior.5
Increase in the trend of childhood obesity has raised a concern in the society.6,7 In this 21st century, the consumption of processed packed foods has seen a rise as people resort to faster availability of food products.8 These food products are high in extrinsic sugar content and preservatives. Sugars are of the following two types: intrinsic sugars and extrinsic sugars. Excessive consumption of extrinsic sugars may predispose individuals to conditions such as obesity, diabetes mellitus, coronary heart disease, hypertension, and other noncommunicable diseases.3
The World Health Organization (WHO) sugar guideline 2015 states that adults and children should reduce their daily intake of sugars to less than 10% of their total energy and a further reduction to 5% would provide additional health benefits. This is in terms of less caries and noncommunicable diseases in terms of obesity. The term “free sugars” was referred to in the 2002 WHO/Food and Agriculture Organization Expert Consultation as “all monosaccharides and disaccharides added to foods by the manufacturer, cook or consumer, plus sugars naturally present in honey, syrups and fruit juices.”9
Behavior is any change observed in the functioning of an organism.10 “Looking at our behavior to determine our attitudes” was rightly said by Eliot Aronson and J. Merrill Carlsmith.11 A child’s dietary health-related behavior is governed by the food consumed and the surrounding environment in the house which is in turn regulated by the parents.12 Reduction in added sugar consumption as a behavior change is needed at the individual as well as a family level. Thus, a study in the form of a 2-week sugar challenge was conducted to assess the behavioral change in families after providing them adequate knowledge regarding the recommended daily amount of sugar required for the proper functioning of the body.
AIM
To assess the dietary behavior change in families participating in a 2-week sugar challenge.
OBJECTIVES
- To assess the willingness of participants to participate in the study.
- To assess the adherence of the families to the challenge at family and individual levels.
- To assess the most commonly consumed food item that led to a failed dietary behavior change.
MATERIALS AND METHODS
Study Design and Setting
This was a cross-sectional, preliminary study which was conducted at a residential complex in Mumbai. The study protocol was analyzed and approved by Institutional Ethics Committee of Yerala Dental College and Hospital, Kharghar, Navi Mumbai. A sample of 30 families were selected for this study.
Participants
The families had children aged 3–12 years and were approached for the challenge, and the ones who were willing to participate were involved in the challenge. Since this study was a preliminary study, a sample size of 30 families was considered adequate.
Inclusion Criteria
- The participants who belonged to American Society of Anaesthesiologists (ASA) categories 1 and 2.
- Those who gave consent for the study.
Since the time sugar was identified as a risk factor for noncommunicable diseases and dental caries, the dietary reduction of the same must be recommended by us. However, dietary behaviors are complex and the choice for the same lies with the family. A family consenting to a certain dietary behavior change “a sugar challenge” was therefore the only inclusion criteria. Healthy families with no obvious need of refined carbohydrates in diet are added.
Exclusion Criteria
- Participants with medical illness or any dietary restrictions.
Study Tool
The study tool comprising a diet chart was given to the participants (Fig. 1) in which they had to mention the food items they could not resist consuming in 2 weeks of challenge period. Using the sugar meter, the participants were informed about the sugar content in 100 g of each of the food items which were not advised to be consumed. Mean and standard deviations of sugar content in 100 g of each item are as follows: biscuits 28.02 ± 10.03, chips and wafers 5.2 ± 3.68, breakfast cereals 16.98 ± 11.11, chocolates 46.86 ± 7.84, fruit juices 26.30 ± 29.98, milk additives 44.161 ± 22.37, soft drinks 12.28 ± 1.39, ice-creams 36.19 ± 28.38, ketchup and jams 39.35 ± 28.69, cakes 27.15 ± 12.97, and Indian sweets 16.25 ± 9.29 per piece13 (Fig. 2). Based on sugar meter (a ready reckoner), the families were asked to self-check the consumption of sugar.
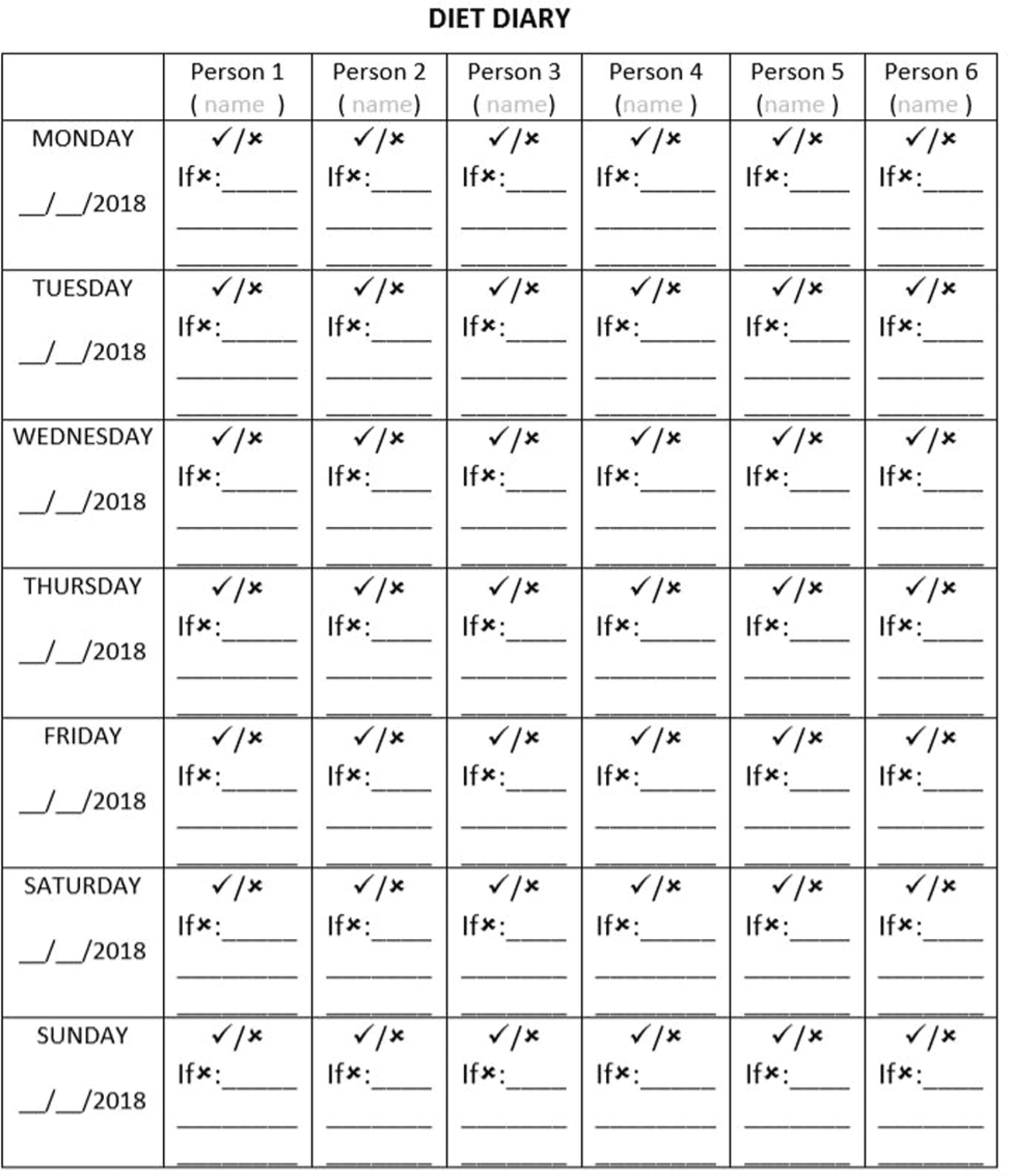
Fig. 1: Diet chart
The challenge was given for 2 weeks from July 25 to August 8, 2018, with a prior intimation of 2–3 days. They were given a list of products that were advised not to be consumed, such as cakes, sweets, ketchup, ice-creams, soft drinks, milk additives, juices, breakfast cereals, chocolates, chips, and biscuits. They were also given a list of products that would benefit their health, in turn leading to a better result of the challenge. They were not provided with any incentive or alternative food products for the same as this would give an incorrect result. The participants were followed up at 1-week and 2-week interval. A reminder was also given regarding the same at the end of first week.
STATISTICAL ANALYSIS
Data were subjected to statistical analysis using the means and standard deviation using MS Excel 2010.
RESULTS
Of the 30 families approached, 25 families were willing to participate in this study as shown in Table 1. Of the total population approached, children showed a complete 100% willingness, whereas only more than 50% of the adults were willing to participate in this study. The enthusiasm of females was found to be more as compared to males in both children and parents in the challenge, as depicted in Table 2. The results that were achieved at the end of the first week showed that a mere 3.13% of children, 2.56% of adults, and 2.81% of individuals could manage to adhere to the challenge. On the contrary, at the end of second week, 3.21% of children, 2.69% of adults, and 2.93% of individuals adhered to the challenge as detailed in Table 3. The most common eaten defaulter food item was milk additives followed by cakes, biscuits, and chocolates as shown in Table 4. The central tendency indicated about 3 days of sustenance of challenge (mean number of days 2.96 and 3.04 and median 2 and 3 for adults and children, respectively) as shown in Figure 3. A detailed analysis revealed that girls showed higher sustainability compared to boys as shown in Table 5.
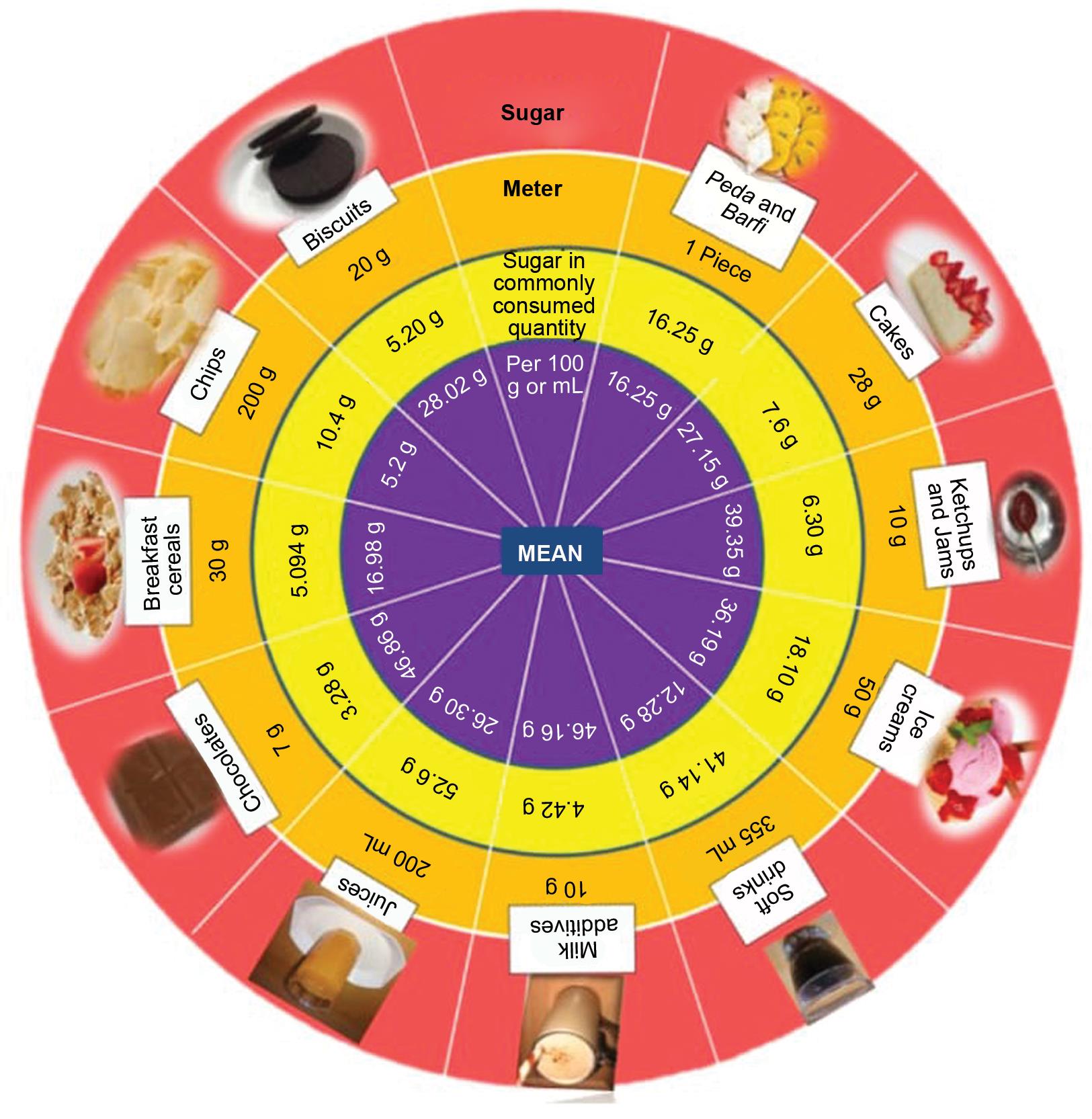
Fig. 2: Sugar meter
| Approached | Participating | |
|---|---|---|
| Families | 30 | 25 |
| Individuals | 103 | 69 |
| Children | 32 | 32 |
| Adults | 71 | 37 |
| Child (%) | Adult (%) | |
|---|---|---|
| Male | 46.90 | 37.50 |
| Female | 53.10 | 62.50 |
| Mean age | 8.78 | 40.12 |
| Children (%) | Adults (%) | Individuals (%) | |
|---|---|---|---|
| Week 1 | 3.13 | 2.56 | 2.81 |
| Week 2 | 3.21 | 2.69 | 2.93 |
| Food items | Percentage of participants consuming it |
|---|---|
| Milk additives | 21 |
| Cakes | 16 |
| Biscuits | 12 |
| Chocolates | 12 |
| Sweets | 9 |
| Ketchup and jams | 8 |
| Ice-creams | 3 |
| Soft drinks | 2 |
| Juices | 7 |
| Cereals | 2 |
| Chips | 8 |

Fig. 3: Distribution of adherence of participants to the challenge
| Adults | Children | Families |
|---|---|---|
| 2.96 (±3.80) | Boys: 2.37 (±2.73) | 0 |
| Girls: 3.74 (±4.55) | ||
| Total: 3.04 (±3.77) |
DISCUSSION
Of the 30 families approached for the study, 5 families were reluctant to participate in the study, the reasons for which were not given by 3 families, and 2 families were certain that they would be not be able to adhere to the challenge. Children showed 100% willingness for the challenge, depicting their profound enthusiasm for the study as they found this concept to be very new and appeared motivated to complete the challenge successfully. On the contrary, adults were unsure of their participation as they found a drastic change in daily routine which was difficult to be adopted. Many adults needed their daily cup of tea or coffee, without which it was difficult for them to begin their day. Also, in adults, females showed higher willingness as compared to males. Males found it difficult to participate in the study as they had to spend a major part of the day outside of the house for work, thus relying on outside food and beverages for hunger needs. The adherence on the part of children was higher compared to adults at week 1 and at week 2, which could be related to the pride of accepting and sustaining the “challenge” being common at young age.14 The adherence seen was low overall in terms of adults and children, as children found consumption of plain milk without sugar to be less palatable as compared to the same milk being consumed with milk additives. Many children also had a habit of eating a bar of chocolate daily without which they did not carry out the required daily work such as going to school or doing their homework. An interesting suggestion received in this study was that the children would show more willingness to consume plain milk without sugar from Monday to Friday and consuming milk with milk additives on Saturdays and Sundays, if given the option. Also, feedback was received at the end of the challenge regarding sweet Sundays, i.e., they could consume sweets once a week on Sundays. They also felt that this initiative of changing their lifestyle was an innovative method and that despite low adherence to the challenge, they were motivated to continue this new schedule later in life. In this study, participants reported sugar cravings that made it difficult for them to adhere to the challenge. This is the only recommendation on sugar guidelines by WHO that adults and children should reduce their daily intake of sugar to less than 10% of their total energy and a further reduction to 5% would provide additional health benefits, hence no age-wise recommendations were provided for intake of dietary sugar.
Habit is an activity carried out at the level of one’s subconscious mind. Thus, in order to break a habit it requires determination, patience, time, and motivation.15 Pediatric dentists have to deal with changing the behavior of children. Behavior change is not easy to achieve and consists of many components for its success.16 Knowledge–attitude–behavior model shows how imparting knowledge to a person causes a shift in attitude, which is responsible for further behavior change.17 However, behavior change is governed by many factors such as surrounding environment, peer pressure, parental practices, genetics, and presence of alternatives and incentives.18,19 The environment in which the child is present plays a very important role in governing the child’s behavior. The amount and type of food available in the house, the type of food consumed by the parents, and the preference for a certain food items by the parents play major roles in governing the children’s eating behaviors.5 Peer influence is another factor affecting behaviors. This was seen in our study where children who participated in the challenge motivated and influenced their friends who also later took up the challenge to adhere to it. Behavioral characteristics of the peer pressure lead to psychological adjustments in children.20
For changing a behavior, a simultaneous change in the routine should be done, which facilitates a smooth behavior change. The most observed reason for not sustaining the challenge was changed “routine”. Based on Charles Duhigg’s model, Cue-Routine-Reward,14 the explanation was provided to participants that change in routine is necessary. Sugar substitution, innovative snacking ideas, and occasional use (sweet Sunday) has changed routines in the past and were recommended to the participants. Although imparting knowledge forms a small part in the process of behavior change, for effective behavior change a more robust technique such as motivational interviewing based on the transtheoretical model of behavior change is necessary. Motivational interviewing uses elicit–change–elicit paradigm as a preferred technique. After initiating a behavior change, certain factors are responsible for the maintenance of the behavior. Initiating an action is the most difficult part of behavior change according to the transtheoretical model.21 A person’s self-motivation plays a major role in initiating and maintaining the changed behavior. Self-determination for continuing an initiated change overpowers the need for incentives or alternatives. People change their dietary behaviors more readily if they have any medical illness or disease that demands such a change compared to those who are not suffering from any illness. Moreover, people driven by the internal locus would accept a behavior or a lifestyle change more readily than those who subscribe to the external locus.22 The dietary patterns of an individual are also regulated by the society and cultural traits and their socioeconomic status.23 Altogether, behavior change is complex and may need myriad interventions.
Our study had limitations such as the sample did not represent all socioeconomic classes. Although the participants of the study were informed about the pros and cons of the sugar-rich food items, no guidance was provided to them throughout the study period. There were neither any incentives for the behavior-change nor alternatives (of food items) suggested.
We claim that the results of the study have generalizability that is limited to similar environments.
CONCLUSION
Willingness in terms of sugar challenge was high but sustainability was poor at the family and at individual levels. The most common consumed food item was milk additives followed by cakes, biscuits, and chocolates.
More research is required in the area of dietary behavior change pertaining to sugar-rich foods.
INSTITUTIONAL ETHICAL CLEARANCE
Ethical clearance was obtained from the Ethics Committee of YMT Dental College and Hospital, Kharghar, Navi Mumbai.
REFERENCES
1. Chi DL, Luu M, Chu F. A scoping review of epidemiologic risk factors for pediatric obesity: Implications for future childhood obesity and dental caries prevention research. J Public Health Dent 2017;77:S8–S31.
2. Heilmann A, Sheiham A, Watt RG, et al. The common risk factor approach-an Integrated population-and evidence-based approach for reducing social inequalities in oral health. Gesundheitswesen 2016;78(10):672–677. DOI: 10.1055/s-0035-1548933.
3. Lustig RH, Schmidt LA, Brindis CD. Public health: toxic truth about sugar. Nature 2012;482(7383):27–29. DOI: 10.1038/482027a.
4. Sheiham A. Improving oral health for all: focusing on determinants and conditions. Health Educ J 2000;59(4):351–363. DOI: 10.1177/001789690005900408.
5. Larsen JK, Hermans RC, Sleddens EF, et al. How parental dietary behavior and food parenting practices affect children’s dietary behavior. Interacting sources of influence? Appetite 2015;89:246–257.
6. WHO. Diet, nutrition and the prevention of chronic disease. Geneva: WHO/FAO Expert Consultation, 2003: (Technical Report Series 916.)
7. Schneider D. International trends in adolescent nutrition. Social Sci Med 2000;51(6):955–967. DOI: 10.1016/s0277-9536(00)00074-5.
8. Antwi F, Fazylova N, Garcon MC, et al. The effectiveness of web-based programs on the reduction of childhood obesity in school-aged children: a systematic review. JBI Libr Syst Rev 2012;10 (Suppl):1–4. DOI: 10.11124/jbisrir-2012-248.
9. World Health Organisation. Guideline: sugars intake for adult and children. Geneva, Switzerland 2015.
10. Damle SG. Textbook of Pediatric Dentistry. Arya Medi Publishing House; 2012.
11. Stangor C. Principles of Social Psychology [Internet]. BCcampus; 2014. Chapter 4, Attitudes Behaviour, And Persuasion. Available from: https://opentextbc.ca/socialpsychology/chapter/changing-attitudes-by-changing-behavior/.
12. Poutanen R, Lahti S, Tolvanen M, et al. Parental influence on children’s oral health-related behavior. Acta Odontol Scand 2006;64(5):286–292. DOI: 10.1080/00016350600714498.
13. Jawdekar AM, Natekar SN, Nagda RJ. Sugar meter-A ready-reckoner tool to inform WHO (2015) sugar guidelines. IDRR 2016;11:16–22.
14. Taylor ZE, Eisenberg N, VanSchyndel SK, et al. Children’s negative emotions and ego-resiliency: longitudinal relations with social competence. Emotion 2014;14(2):397. DOI: 10.1037/a0035079.
15. Charles D. The Power Of Habit [Internet] The Random House Publishing Group. 2011 - [cited 2012]. Available from: http://takechargeworld.com/wp-content/uploads/2016/09/Charles-Duhigg.The-Power-of-Habit.pdf.
16. Michie S, Ashford S, Sniehotta FF, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011;26(11):1479–1498. DOI: 10.1080/08870446.2010.540664.
17. Bettinghaus EP. Health promotion and the knowledge-attitude-behavior continuum. Prev Med 1986;15(5):475–491. DOI: 10.1016/0091-7435(86)90025-3.
18. Tolvanen M, Anttonen V, Mattila ML, et al. Influence of children’s oral health promotion on parents’ behaviours, attitudes and knowledge. Acta Odontol Scand 2016;74(5):321–327. DOI: 10.3109/00016357.2015.1122836.
19. Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin 2001;48(4):893–907. DOI: 10.1016/s0031-3955(05)70347-3.
20. Prinstein MJ, Boergers J, Spirito A. Adolescents’ and their friends’ health-risk behavior: factors that alter or add to peer influence. J Pediatr Psychol 2001;26(5):287–298. DOI: 10.1093/jpepsy/26.5.287.
21. Horwath CC. Applying the transtheoretical model to eating behaviour change: challenges and opportunities. Nutr Res Reviews 1999;12(2):281–317. DOI: 10.1079/095442299108728965.
22. Hochbaum G, Rosenstock I, Kegels S. Health belief model. United States Public Health Service 1952.
23. Popkin BM. Nutritional patterns and transitions. Popul Dev Rev 1993;19(1):138–157. DOI: 10.2307/2938388.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.